Testing for hepatitis C could save your life

If a simple blood test could improve your long-term health or possibly save your life, would you have it performed? The answer for most people is a resounding yes.
Testing for hepatitis C, which involves a basic blood draw and analysis, can be the difference between serious health complications later in life or a manageable condition that is curable in most cases when it's treated.
Here are answers to common questions about chronic hepatitis C:
What is hepatitis C?
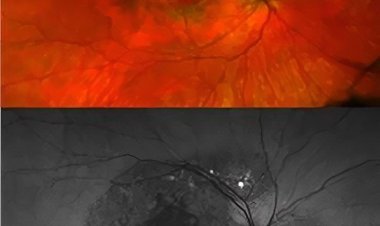
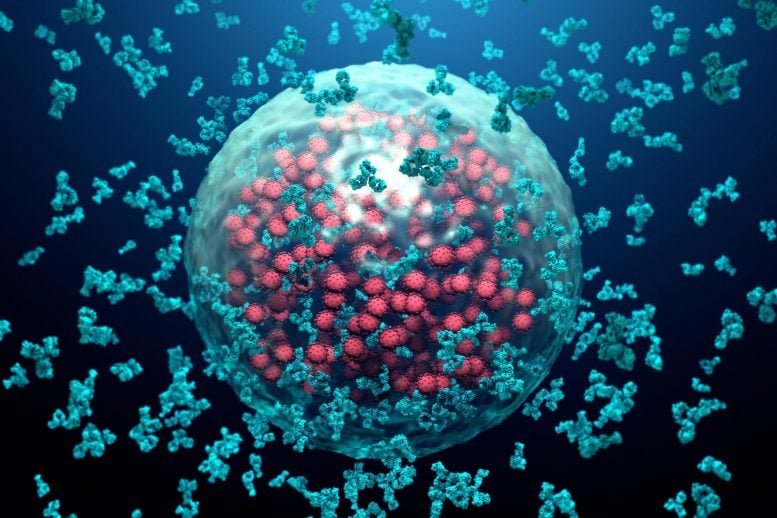
Hepatitis C is a viral infection that targets the liver, leading to inflammation and scarring if untreated. Of the several hepatitis viruses, hepatitis C is one of the most severe forms. Hepatitis A, hepatitis B, hepatitis C and hepatitis E are different diseases.
Passed through contact with contaminated blood, hepatitis C is often contracted by sharing contaminated needles or snorting drugs. However, receiving a blood transfusion, clotting factor or organ transplant before 1992, getting piercings or tattoos in an unsterile environment, and having a history of incarceration also are risks for contracting hepatitis C.
What are the symptoms of hepatitis C?
Many people with hepatitis C don't know they are infected. Symptoms typically don't appear until years later in the course of chronic infection.
Signs of chronic infection include:
- Bleeding easily
- Bruising easily
- Itchy skin
- Fluid accumulation in your abdomen
- Swelling in the legs
- Weight loss
- Confusion, drowsiness and slurred speech
- Spiderlike blood vessels on your skin
Because symptoms usually don't appear until after hepatitis C has caused years of liver damage, the importance of screening is vital.
Who should be tested for hepatitis C?
Consider a hepatitis C test if you:
- Were born between 1945 and 1965. This population includes the highest rate of infection in the general public
- Have injected or snorted drugs — current user or history of use
- Had gotten a tattoo in an unprofessional or unsterile environment
- Were incarcerated
- Received a blood transfusion, organ transplant or clotting factor before 1992
As of March 2020, the U.S. Preventive Services Task Force recommends screening for all adults aged 18–79.
Talk to your health care professional if you have questions or concerns about being tested for hepatitis C.
What are the potential complications of hepatitis C?
Left untreated or undetected, hepatitis C can cause serious complications, such as:
- Cirrhosis (scarring) of the liver tissue, which impedes the liver function
- Liver cancer
- Liver failure
Is treatment available for hepatitis C?
Again, diagnosing hepatitis C infection early is integral to optimal long-term health. Antiviral medications are available to treat and eliminate hepatitis C from your body.
Older forms of these medications, which required patients to be on a regimen for 24–72 weeks, often elicited serious side effects, including depression, flu-like symptoms and loss of healthy blood cells. On the other hand, new antiviral medications are oral pills with a low risk of side effects and much better cure rates. New therapies also can be as short as eight weeks.
Overall, the new treatments are superior to older agents, which excluded people with mental illness or a history of suicide. Newer agents have few exclusion criteria. People who were barred from treatment in the past now can possibly be treated and cured. If people underwent treatment in the past and were not cured, they should be reevaluated.
Your health care team may recommend lifestyle changes to keep you and others healthy if you are diagnosed with hepatitis C. Common measures are refraining from consuming alcohol, avoiding medications that may cause liver damage and taking extra precautions to protect others from contact with your blood.
If you're at risk of hepatitis C, talk to your health care professional about testing. Identifying and treating health issues early can improve your well-being for years to come.